10 Counselling & Therapy Myths Your Friends Believe
Rod Mitchell, MSc, MC, Registered Psychologist
Key Highlights
Over 60% of people avoid therapy due to stigma, yet 21%+ of adults use it for everyday stress, relationships, and growth - not just severe illness.
Effective therapy matches treatment approaches - CBT for thought patterns, EMDR for trauma, or DBT for emotion regulation - to your specific concerns and goals.
Most people see meaningful improvement within 10-15 sessions for specific issues, though complex trauma may take 12-18 months of appropriate work.
When clients first contact me about starting therapy, they often preface their concerns with qualifying statements: "I know my problems aren't that serious," "I should probably be able to handle this on my own," or "Maybe I'm just being weak." These hesitations reveal how deeply therapy myths shape people's decisions about seeking support - often keeping them struggling alone with issues that therapy could effectively address.
This article examines ten common myths about therapy - from concerns about weakness and cost to confusion about what actually happens in sessions - and provides the clinical reality behind each one. You'll gain an insider's perspective on the therapeutic process, understand when and why therapy works (and when it might not), and have the information needed to make informed decisions about whether therapy could support your goals.
Once you've moved past common therapy myths, understanding the practical differences between treatment approaches becomes crucial. Our article "Counselling vs Therapy: Choose Wrong & Waste Months (Avoid This)" helps you select the right type of support for your specific situation, potentially saving you significant time and money.
Table of Contents Hide
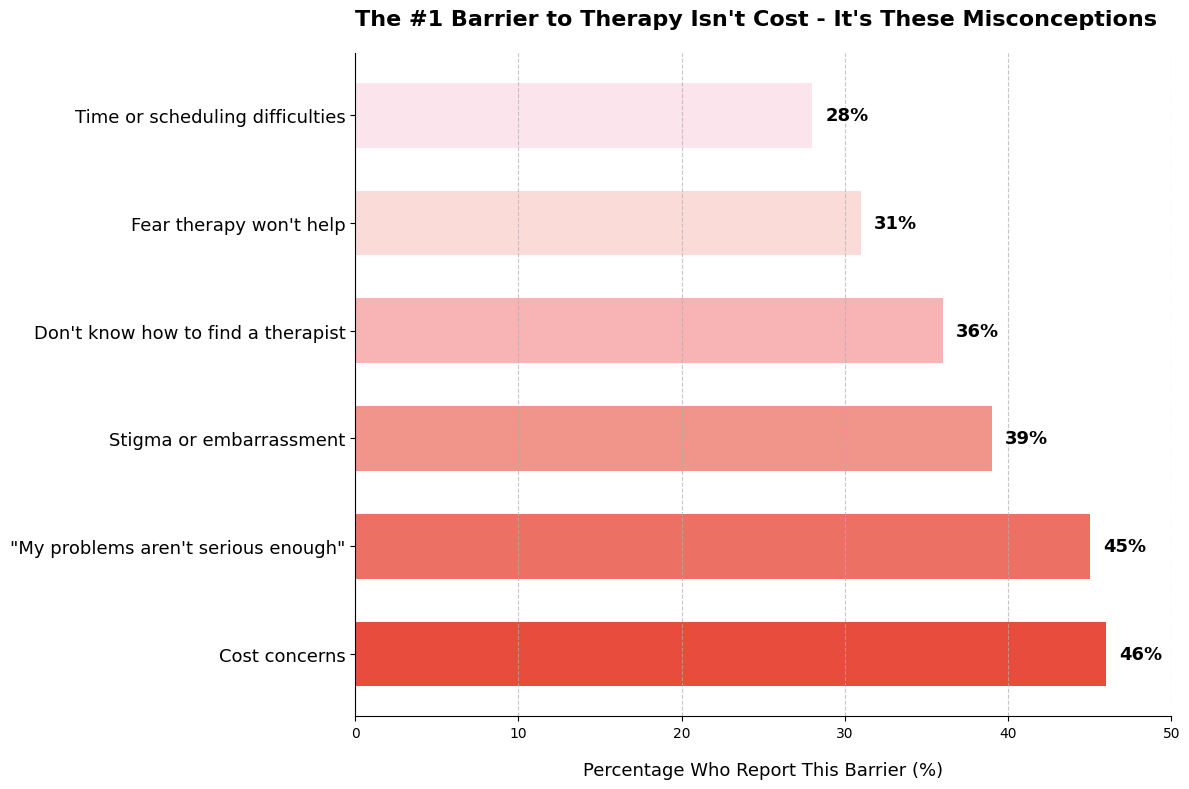
When researchers ask what stops people from starting therapy, the answers reveal something surprising: The top two barriers aren't about logistics - they're about mindset. Nearly half (45%) think their problems "aren't serious enough," while 39% cite stigma or embarrassment. Cost does matter (46%), but when you combine the psychological barriers, they outweigh practical concerns nearly 2-to-1.
This explains why simply making therapy more affordable hasn't eliminated the treatment gap. For many people, the biggest obstacle isn't finding the money or time - it's giving themselves permission to ask for help.
Myth #1: "Therapy Is Only for People With Severe Mental Illness"
The assumption that therapy is reserved for crisis situations keeps many people from seeking support that could meaningfully improve their lives.
More than 21% of adults use therapy services. The majority aren't in crisis - they're managing everyday stress, navigating life transitions, or working on personal growth.
Research reveals that 40-50% of people accessing therapy don't meet criteria for diagnosable mental disorders. They're addressing concerns like relationship friction, career uncertainty, parenting challenges, or the chronic stress of juggling multiple responsibilities.
What Therapy Actually Addresses
People seek therapy for a wide range of human experiences:
Work transitions: Managing promotion stress, career changes, or professional identity questions
Relationship concerns: Improving communication, navigating conflict, or strengthening connection
Life adjustments: Processing grief, adapting to major changes, or finding meaning during transitions
Personal development: Building confidence, clarifying values, or developing emotional awareness
Stress management: Learning coping strategies before burnout becomes crisis
These aren't trivial concerns. A parent struggling to connect with their teenager during a difficult transition, or a professional managing the anxiety of new leadership responsibilities - these situations create real distress and benefit from therapeutic support.
Prevention Works Better Than Crisis Intervention
Waiting until problems become severe isn't just unnecessary - it's often counterproductive.
Studies show that early intervention for mild symptoms reduces the likelihood of developing clinical disorders by 40-50%. Norway's healthcare system recommends therapy as first-line treatment for mild depression, achieving 65% remission rates compared to 35% spontaneous remission in those who wait.
People who address concerns early typically need 8 sessions to see meaningful improvement. Those who wait until symptoms are severe often require 18 sessions to achieve comparable outcomes.
Some of my most meaningful clinical work happens with clients managing everyday challenges rather than diagnosable conditions. A client learning to set boundaries with demanding family members, or someone processing the identity shift of becoming a parent for the first time - these situations involve genuine growth and change.
The therapeutic process is fundamentally the same whether someone is addressing clinical depression or navigating a significant life transition. We use the same evidence-based techniques, build the same quality of therapeutic relationship, and work toward comparable goals of increased wellbeing and effective functioning.
"Early intervention not only prevents escalation to clinical disorders in about half of cases, but also reduces overall treatment burden when problems do develop." - Dr. Pim Cuijpers, Professor of Clinical Psychology
If you're wondering whether your concerns are "serious enough" for therapy, consider this: therapy isn't about meeting a severity threshold - it's about getting support for challenges that matter to you.
Myth #2: "Going to Therapy Means You're Weak"
The fear of appearing weak keeps more people from therapy than any other single barrier.
Research shows that over 60% of people cite shame or stigma as a reason they avoid seeking mental health support. This isn't about whether therapy works - it's about what seeking help might mean about them.
The narrative that therapy signals weakness gets the reality exactly backward. Consider the high-performing professional who recognizes their stress is affecting their relationships and actively seeks strategies to address it. Or the parent who notices they're repeating unhelpful patterns from their own childhood and wants to break the cycle.
These decisions require self-awareness, honesty, and the courage to acknowledge that struggling doesn't mean failing.
Seeking therapy demonstrates several strengths: the self-awareness to recognize when something isn't working, the resourcefulness to pursue solutions rather than hoping problems resolve on their own, the humility to admit you don't have all the answers, and the commitment to invest time and effort into personal growth.
People who avoid therapy often do so not because they're stronger, but because confronting difficult emotions or patterns feels too threatening. Avoidance is the easier path. Engagement takes courage.
Identity-Specific Barriers to Seeking Help
Stigma doesn't affect everyone equally. Certain groups face additional layers of judgment around mental health support.
Men face socialization against vulnerability. Traditional masculinity norms emphasize self-reliance and emotional stoicism. Admitting you need help can feel like violating deeply ingrained expectations about what it means to "be a man."
Some cultural communities experience heightened therapy stigma. In cultures that prioritize family privacy or view mental health struggles as bringing shame to the family, seeking outside help can feel like a betrayal of cultural values.
LGBTQ+ individuals may need affirming therapy. Past experiences with judgment or misunderstanding can make seeking help feel risky. Finding a therapist who understands your identity matters deeply.
These barriers are real, and acknowledging them isn't about reinforcing stereotypes - it's about recognizing that the decision to seek therapy happens within complex social contexts.
In my practice, I consistently observe something striking about clients who take the step to start therapy. They demonstrate more self-awareness than many people who struggle alone.
They've already done the difficult work of recognizing a pattern they want to change. They've moved past defensiveness or denial to honest assessment.
That's not weakness. That's courage in action - the kind that leads to actual change rather than years of avoidance.
If you're hesitating about therapy because of what it might say about you, consider: seeking support when you need it is what strong, self-aware people do.
Myth #3: "Therapy Is Just Talking - It Doesn't Really Help"
The phrase "just talking" fundamentally misrepresents what happens in effective therapy.
Research on cognitive behavioral therapy shows that 60-75% of people with anxiety and depression see significant improvement after structured treatment. These aren't results from casual conversation - they come from active, evidence-based techniques practiced systematically over time.
What Different Therapies Actually Do in Sessions
| Therapy Type | What Happens in Sessions | Best For |
|---|---|---|
| CBT | Track thought patterns in written records, test assumptions through behavioral experiments, build exposure hierarchies for feared situations | Anxiety, depression, panic |
| EMDR | Process traumatic memories while following bilateral stimulation (eye movements, tapping), reprocess stored trauma responses | PTSD, trauma, disturbing memories |
| EFT (couples) | Identify attachment patterns, practice vulnerability in guided conversations, repair specific relationship injuries | Relationship disconnection, conflict cycles |
| CART | Map anger triggers, practice regulation techniques with biofeedback, track patterns between sessions | Anger management, emotional reactivity |
Consider someone with social anxiety about an upcoming presentation. In CBT, we wouldn't just discuss their fear - we'd identify specific catastrophic thoughts ("I'll forget everything and everyone will think I'm incompetent"), examine evidence for and against those predictions, and practice the presentation in graduated steps.
How Sessions Actually Work
First session focuses on assessment. We explore what brought you in, identify specific goals, discuss relevant history, and create a treatment plan together.
Ongoing sessions follow a structured pattern. We check in briefly, focus on your primary goal for that session, practice specific techniques actively, and assign between-session work.
This isn't passive listening. You're learning skills and applying them immediately.
Between sessions, you practice what we've worked on. This might include:
Tracking thought patterns or emotional triggers
Practicing specific regulation techniques
Completing behavioral experiments
Implementing new communication strategies
Progress gets measured through regular check-ins about your goals and standardized outcome measures, not subjective feelings alone.
When I work with clients on anger management using CART, we don't just talk about anger abstractly.
We map their specific triggers in detail - exactly what situations, thoughts, or physical sensations precede their reactive episodes. We practice regulation techniques in session, sometimes using biofeedback to see their nervous system respond in real-time.
They track patterns between sessions using structured logs. It's systematic, measurable work with clear skills being built progressively.
The therapeutic relationship is collaborative. I'm not telling you what to do - I'm teaching you techniques, helping you understand patterns, and supporting you in making informed decisions aligned with your values and goals.
You're an active participant, not a passive recipient. The work happens through your engagement, practice, and application of what we explore together.
Myth #4: "Therapy Takes Years to Work"
The belief that therapy requires indefinite commitment keeps people from starting altogether.
Research tracking therapy outcomes shows that 50% of people experience meaningful recovery after 15-20 sessions. For many specific concerns, you'll notice changes much sooner.
Timeline Varies by What You're Working On
Short-term, focused therapy addresses specific issues efficiently:
Recent stress or transitions: 8-12 sessions for someone navigating a career change or relationship adjustment
Specific anxiety: 12-16 weeks of CBT for panic attacks or social anxiety
Acute grief: 10-15 sessions processing a significant loss
Communication skills: 8-12 couples sessions learning conflict resolution
Someone managing anxiety about returning to work after parental leave might see substantial improvement within three months of weekly sessions.
When Therapy Takes Longer - and Why That Makes Sense
More complex situations appropriately require extended work. This isn't because therapy is ineffective - it's because deep change takes time.
Chronic conditions like depression with multiple relapses might need 12-18 months to build lasting coping strategies and address underlying patterns. Complex trauma involving childhood experiences requires careful processing that can't be rushed safely.
Co-occurring issues - anxiety alongside substance use, or depression complicated by chronic pain - need integrated treatment addressing multiple concerns simultaneously.
Research shows an interesting pattern: about 50% of people improve significantly by session 8, and 75% by session 26. But gains continue with additional sessions for those working on deeper concerns.
Therapy duration depends heavily on what you want to work on. Someone managing anxiety about public speaking might see meaningful progress in 8-12 sessions.
Someone processing childhood trauma might work with me for a year or more. Both timelines are appropriate for their respective goals.
Several factors affect how quickly you'll see progress: the severity and duration of your concerns, consistency in attending sessions and practicing between them, how well the therapeutic approach matches your needs, and the complexity of what you're addressing.
The most important element: open dialogue with your therapist about progress. You should feel comfortable asking "Are we making progress at a reasonable pace?" or "How will we know when we're done?"
A good therapist welcomes these conversations and works collaboratively with you to assess whether the timeline and approach are working for your specific situation.
Myth #5: "A Therapist Will Just Tell Me What to Do"
One of the most common misconceptions is that you'll explain your problem and the therapist will hand you the solution.
That's not how effective therapy works.
Therapists function as guides, not advice columnists. Research shows that the therapeutic relationship - characterized by collaboration and genuine partnership - predicts outcomes far more than the specific techniques used.
What Therapists Don't Do vs. What They Actually Do
| Therapists Don't | Therapists Do |
|---|---|
| Tell you what decision to make about your job, relationship, or life path | Help you examine what matters most to you and how different choices align with your values |
| Impose interpretations about what your experiences mean | Ask questions that help you discover your own insights about patterns and motivations |
| Assign homework you have no say in | Collaboratively design action steps based on your goals and what feels manageable |
| Continue with their agenda when you show signs of disagreement | Constantly check whether their observations resonate with your experience |
You're the expert on your own life - your history, values, circumstances, and what feels right for you. The therapist brings expertise in understanding patterns, teaching coping strategies, and helping you see options you might not have considered.
Think about someone struggling with whether to stay in a demanding career. A therapist won't say "quit" or "stick it out."
Instead, we explore: What makes this work meaningful or draining? How does this situation connect to larger patterns in your life? What would staying or leaving look like six months from now? What values are competing here?
You make the decision. The therapist helps you understand all the factors involved so that decision feels informed rather than reactive.
Your Agency in the Process
Effective therapy preserves and strengthens your autonomy.
When we discuss practice exercises, you're involved in deciding what makes sense to try. If I suggest tracking anger triggers daily and you know that won't happen given your schedule, we'll adjust the approach together.
"The therapist is not a technician who applies interventions to passive recipients. Therapists who can form strong alliances while respecting client agency produce consistently better outcomes than those focused primarily on technique delivery." - Dr. Bruce Wampold, Professor of Counseling Psychology
My role isn't to tell clients whether to repair a struggling marriage or leave it. It's to help them understand their attachment patterns, communication dynamics, and what they genuinely want from intimate relationships.
I help them see their options clearly, including consequences they might not have considered. But the decision - and the responsibility for that decision - remains theirs.
This preserves something crucial: your sense of ownership over your own life. Change that you choose for yourself tends to stick far better than change imposed by someone else, even a well-meaning therapist.
If you're looking for someone to tell you exactly what to do, therapy might feel frustrating at first. But what you gain is far more valuable: clarity about who you are and what matters to you, skills to navigate difficult decisions, and confidence in your own judgment.
Myth #6: "I Can Just Talk to Friends or Family Instead"
Both therapy and social support matter for wellbeing, but they serve fundamentally different purposes.
Friends and family provide emotional connection, shared experiences, and the comfort of being known. These relationships sustain us through everyday challenges and remind us we're not alone.
Therapy offers something else entirely: a professional relationship specifically designed for psychological work.
How Therapy Differs From Social Support
Professional boundaries enable deeper disclosure. Research shows that 83% of therapy clients discuss topics they've never shared with anyone else. The one-directional nature - where you don't need to manage the therapist's reactions or worry about burdening them - creates safety for difficult conversations.
Trained interventions target specific patterns. A friend might offer comfort when you're anxious. A therapist teaches you concrete regulation techniques, helps you identify thought patterns fueling the anxiety, and creates structured exposure plans.
Confidentiality protects your privacy. What you discuss stays in the therapy room. There's no risk of your struggles becoming known in your social circle or affecting how others see you.
No reciprocity required. You don't need to take care of your therapist's feelings, ask about their week, or worry whether you're taking up too much space. The relationship exists solely for your benefit.
Think about a friend trying to support someone through complicated grief. They can listen, validate, and sit with the pain. That matters deeply.
But they likely can't help that person understand how their grief connects to earlier losses, teach them specific strategies for managing grief waves, or know when the grief has shifted into clinical depression requiring different intervention.
Cultural Considerations
In some cultural contexts, seeking help outside the family feels particularly difficult. Communities that emphasize family privacy or view personal struggles as bringing shame to the family create a painful bind - people suffer silently to protect family honor.
Research shows that 73% of individuals in collectivist cultures report reluctance to burden family members with psychological distress. The expectation to handle problems privately can delay help-seeking for years.
In my practice, I've worked with clients from cultural backgrounds where discussing emotional struggles outside the family violates deeply held values. Therapy offers them a confidential space that doesn't require disclosing family matters to friends or extended community.
The privacy of the therapeutic relationship becomes especially valuable when cultural norms make vulnerability feel like betrayal.
Dr. Bruce Wampold, psychotherapy researcher, explains the essential distinction: "Therapy works through the systematic application of psychological principles within a healing context. While friends provide comfort and connection, therapists deploy specific strategies that restructure how people process experience. The therapeutic relationship isn't better than friendship; it's functionally different, designed for change rather than continuity."
This doesn't diminish the value of social support. Friends and family remain essential for connection, belonging, and everyday coping.
But when you're facing patterns that persist despite support from loved ones, when you need skills you don't currently have, or when discussing your struggles feels unsafe in your existing relationships - that's when the specific structure of therapy becomes necessary.
You don't have to choose between therapy and social support. Most people benefit from both, each serving its distinct and valuable purpose.
Myth #7: "All Therapy Is the Same"
Walking into therapy isn't a one-size-fits-all experience.
Different therapeutic approaches use fundamentally different techniques, focus on different aspects of your experience, and suit different types of concerns. The quality of fit between you and your therapy approach accounts for up to 30% of your outcomes - often more than the therapist's years of experience.
Common Therapy Types and What They Actually Do
| Approach | Focus | Works Best For |
|---|---|---|
| CBT | Changing thought patterns and behaviors through structured exercises | Anxiety, depression, panic, specific fears |
| Psychodynamic | Exploring unconscious patterns and how past experiences shape present relationships | Relationship patterns, self-understanding, personality concerns |
| EMDR | Processing traumatic memories through bilateral stimulation | PTSD, single-incident trauma, disturbing memories |
| DBT | Building skills for emotion regulation and distress tolerance | Intense emotions, self-harm, borderline personality disorder |
| EFT | Reshaping emotional responses and attachment patterns in relationships | Couples therapy, relationship disconnection |
Someone who prefers structured, concrete steps might thrive in CBT but feel frustrated by the open-ended exploration of psychodynamic therapy. Conversely, someone seeking deeper self-understanding might find brief CBT protocols too surface-level.
Therapy Structures Beyond Individual Sessions
Format matters as much as approach:
Individual therapy: One-on-one work on your specific concerns
Couples therapy: Focused on relationship patterns and communication
Family therapy: Addresses family dynamics and system-level patterns
Group therapy: Shared learning and support with others facing similar challenges
Research shows that when people receive their preferred therapy type, dropout rates fall from 35% to 18%. Fit matters independently of how skilled your therapist is.
In my practice, I've observed that clients can usually sense within the first two to three sessions whether the therapeutic approach resonates with how they naturally think and solve problems.
This isn't about the therapist being "good" or "bad" - it's about whether the framework matches their needs. Someone who wants immediate tools for managing panic attacks will respond differently than someone wanting to understand why they keep choosing unavailable partners.
Dr. Bruce Wampold, psychotherapy researcher at the University of Wisconsin-Madison, explains: "Clients can sense within the first two to three sessions whether the therapeutic approach resonates with their worldview and problem-solving style. This felt sense of fit predicts outcomes more powerfully than therapist experience level."
Finding the right therapeutic approach means asking potential therapists about their methods, being honest about what you're looking for, and trusting your sense of whether the framework feels helpful or confusing.
If something feels off after a few sessions, that's valuable information - not a sign that therapy doesn't work, but that a different approach might serve you better.
Myth #8: "Therapy Is Too Expensive and Inaccessible"
Cost creates real barriers to mental health care.
Acknowledging this reality isn't pessimistic - it's the starting point for finding practical solutions that work within your actual constraints.
The landscape of therapy access has changed significantly. During 2020, 80% of mental health visits shifted to remote delivery, and research shows telehealth maintains effectiveness comparable to in-person treatment for most conditions. This expansion, combined with underutilized workplace benefits and community resources, creates more pathways to affordable care than many people realize.
Practical Options for Accessing Affordable Therapy
Check what you already have access to:
Extended health benefits: Many workplace plans cover 500-3000 dollars annually for therapy. Call the number on your insurance card and ask specifically about mental health coverage, per-session limits, and whether you need referrals.
Employee Assistance Programs (EAP): Research shows 70-85% of employees don't know their employer offers EAPs, which typically provide 3-8 free confidential counseling sessions. Check your employee handbook or HR portal.
Sliding scale fees: Many therapists reserve slots for reduced-fee clients. Ask directly: "Do you offer sliding scale rates based on income?" Some practices offer 20-40% reductions for financial need.
Community mental health centers: Federally qualified health centers accept clients regardless of ability to pay. Calgary Counselling Centre and other community agencies provide services on sliding scales starting as low as $30-50 per session.
University training clinics: Graduate programs offer supervised therapy at significantly reduced rates (often $10-50 per session). University of Calgary and other institutions run training clinics with therapists-in-training under expert supervision.
Group therapy: Sessions typically cost $30-80 per person compared to $100-200 for individual therapy, while research shows 75-85% of individual therapy effectiveness for conditions like depression and anxiety.
Telehealth Expands Geographic Access
Remote therapy removes transportation barriers and wait times.
You can work with therapists across Alberta rather than limiting yourself to your immediate area. Research tracking 2,000 patients transitioning to telehealth found that 73% maintained equivalent clinical outcomes, with particular success for anxiety and mood disorders.
The question isn't whether therapy costs money - it does. The question is whether the accessible options available can fit your situation and budget when you know where to look.
Start with what you have access to right now: your benefits, your employer's EAP, or community resources in your area. Many people find affordable therapy exists closer than they initially thought.
Myth #10: "If Therapy Doesn't Help Right Away, It Means It Won't Work"
Therapy is powerful, but it's not universal.
Assuming early struggles mean permanent failure misses important nuances about fit, timing, and readiness. But the reverse assumption - that therapy will definitely work if you just stick with it - also oversimplifies reality.
Sometimes therapy doesn't work because you haven't found the right approach yet. Sometimes the timing isn't right. And sometimes therapy genuinely isn't the answer for what you're facing right now.
When Therapy May Not Be First-Line Treatment
Certain situations require stabilization or different interventions before therapy becomes productive:
Active psychosis or mania: Psychiatric stabilization needed before talk therapy
Acute safety crisis: Immediate intervention takes priority
Severe substance dependence: May need medical detox first
Coerced participation: Someone forced into therapy often isn't ready for change work
These aren't therapy failures. They're situations where other interventions come first.
What "Therapy Not Working" Often Signals
When therapy feels ineffective, it usually points to mismatch rather than therapy being useless:
Wrong modality: You're doing CBT for complex trauma but need EMDR, or talk therapy for ADHD when you need skills coaching
Wrong therapist fit: Personality mismatch, communication style doesn't resonate, or cultural understanding gaps
Timing issues: External crisis demanding attention, or you're not ready for change yet
Need additional support: Therapy alone isn't enough - medication evaluation, medical care, or peer support may help
Normal therapeutic discomfort: Growth feels uncomfortable; distinguish this from feeling misunderstood or invalidated
In my practice, I've seen therapy "not work" for various reasons.
Sometimes a client needs EMDR for trauma but they're in standard CBT. Sometimes they're not ready yet and return six months later when circumstances shift.
Sometimes we're a personality mismatch and another therapist is better fit. None of these mean therapy doesn't work - they mean finding the right fit and approach matters.
"Clients who understand therapy as hard work that takes time do better than those expecting a therapist to 'fix' them quickly. Setting realistic expectations - including that symptoms might temporarily worsen as difficult issues surface - prevents dropout." - Dr. Michael Lambert, psychotherapy researcher
Talk openly with your therapist about concerns. A good therapist welcomes this conversation without defensiveness.
Questions to explore: Is this the right approach for what I'm working on? Are we addressing my actual priorities? Do I need something additional? Research shows that when clients discuss fit concerns directly, outcomes improve in about two-thirds of cases through collaborative problem-solving.
If your therapist becomes defensive when you raise concerns, that's valuable information about fit.
Sometimes the bravest decision is recognizing therapy isn't the right tool right now. That's not failure - it's self-awareness about what you actually need.
Conclusion
The myths we've examined - from believing therapy is only for crisis to fearing it takes years - create unnecessary distance between people and support that could meaningfully improve their lives.
Understanding what therapy actually involves, who it serves, and how to assess whether it's working removes the fear-based barriers that keep people struggling alone with challenges that effective treatment could address.
If You're Considering Therapy
Think about what you'd want to work on. Research shows people who articulate specific goals achieve better outcomes than those starting with vague aims.
Maybe you're managing stress that's affecting your sleep and relationships. Perhaps you recognize patterns you want to change - reacting intensely to criticism, avoiding difficult conversations, or feeling disconnected in your relationships.
You don't need a crisis or diagnosis to benefit from therapy. You need genuine concern about something in your life and willingness to work on it.
Don't let myths hold you back from exploring options. The courage to challenge misconceptions and seek support represents strength and self-awareness, not weakness.
Studies show that people who complete structured self-assessments before deciding about therapy are 34% more likely to seek appropriate help compared to those relying on informal evaluation alone.
Practical Next Steps
Finding and starting therapy involves several concrete actions:
Ask your doctor for referrals based on your specific concerns and insurance coverage
Search psychologist directories like Psychology Today or the College of Alberta Psychologists directory, filtering by specialty and location
Complete phone consultations with 2-3 potential therapists to assess fit, asking about their approach, experience with your concerns, and treatment structure
Evaluate fit by the third session - you should feel heard, sense genuine therapist interest, and feel comfortable being honest about concerns
Discuss progress openly with your therapist throughout treatment; good therapists welcome conversations about whether the approach is working
Remember therapy is collaborative work where you're an active participant, not a passive recipient. The relationship and your engagement matter as much as the techniques used.
One pattern I consistently observe: clients who finally start therapy often say within the first month, "I wish I'd done this years ago." What they're recognizing isn't that their earlier struggles were invalid, but that support was available and effective all along.
The myths kept them waiting - believing their problems weren't serious enough, that therapy meant weakness, or that it wouldn't actually help.
If you're in Calgary and looking for support with anger, trauma, relationships, or anxiety, my practice at Emotions Therapy Calgary offers evidence-based treatment tailored to your specific goals.
If you're experiencing crisis or thoughts of self-harm, please reach out immediately - don't wait. Call the Calgary Distress Centre at 403-266-4357, the 988 Suicide Crisis Helpline, or text a crisis line. You deserve support, and help is available right now.