How to Calm Down: What 10+ Years Treating Anxiety Taught Me
Rod Mitchell, MSc, MC, Registered Psychologist
Key Highlights
Roughly 20-30% of people experience increased anxiety with deep breathing - this is a normal nervous system response, not failure.
Effective anxiety counselling matches techniques to your nervous system: breathing methods, body-based regulation, movement approaches, or cognitive reframing strategies.
Your autonomic nervous system has a "brake" called the vagal nerve that breathing, humming, and cold water activate to reduce stress.
With practice, most people identify 2-3 go-to calming techniques that consistently work for their unique nervous system within several weeks.
In over a decade of treating anxiety, I've noticed something that surprises most new clients: the "just breathe" advice they've heard countless times can actually make their panic worse. This isn't a personal failing - it's a normal nervous system response that roughly 20-30% of people experience when they're not accustomed to focusing inward during distress.
Understanding how to calm down effectively isn't about forcing yourself through techniques that don't match your nervous system. Research on emotion regulation shows that different emotional states - and different people - require fundamentally different approaches. What works brilliantly for anxiety might amplify anger, and what grounds one person might leave another feeling more activated.
This article walks you through:
The most effective calming techniques based on neuroscience and clinical practice
Which approaches match your specific emotional state and nervous system wiring
What to do when standard techniques aren't working
If you're also struggling with persistent anxiety, our article on “The 5 Best Types of Therapy for Anxiety” explores professional treatment options in depth.
Table of Contents Hide
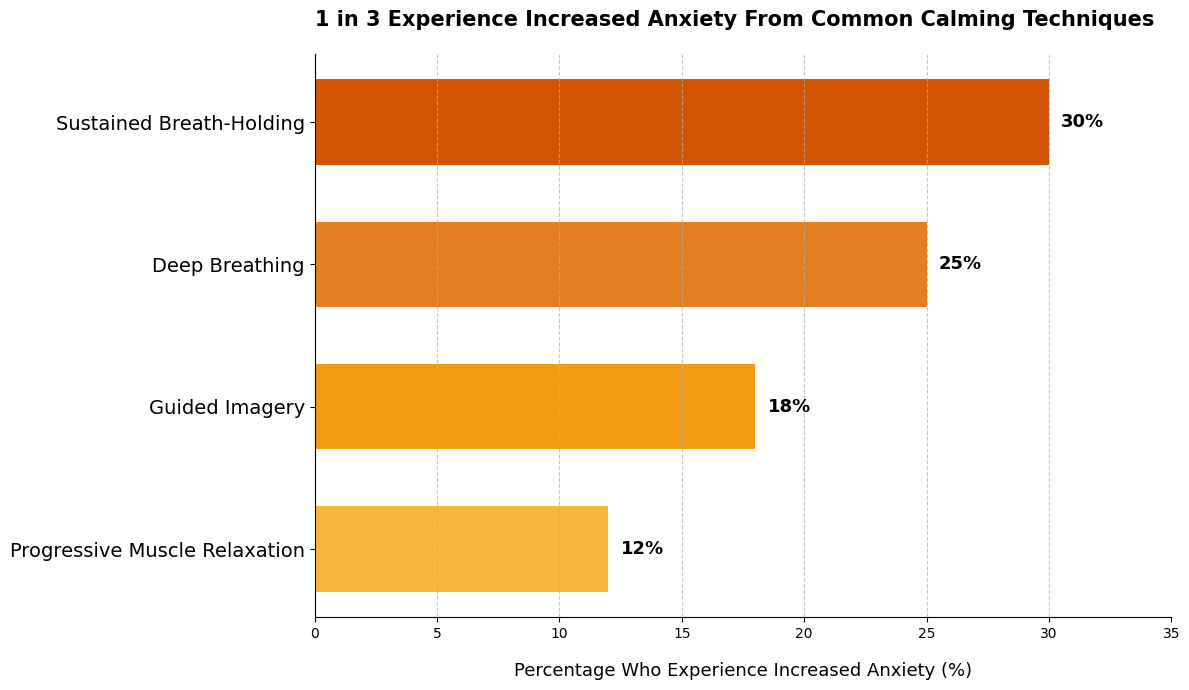
Between 12% and 30% of people experience increased anxiety, unwanted thoughts, or emotional distress when attempting common calming techniques - not because they're "doing it wrong," but due to individual differences in trauma history, nervous system sensitivity, and current activation level.
Progressive muscle relaxation has the lowest paradoxical response rate (12%), while techniques involving breath control show higher rates. If a calming technique makes you feel worse, that's information about what your nervous system needs right now, not a personal failure.
Why Breathing Doesn't Always Work
Here's something most advice skips: slow breathing can actually make your panic worse.
Research shows that 15-20% of people experience increased anxiety during deep breathing exercises. This isn't failure - it's your nervous system responding to an unfamiliar sensation of focusing inward when you're already on high alert.
Why breathing typically works: Your vagus nerve acts as your nervous system's brake pedal. Slow, deep breathing activates this nerve, telling your body to shift from fight-or-flight into rest mode. Heart rate drops, blood pressure lowers, stress hormones decrease.
But for some people, the sensation of slowing down triggers more panic. Their brain interprets the body changes as dangerous rather than calming.
In my practice, I've observed that roughly 20-30% of clients initially experience heightened anxiety with deep breathing. This happens most often with people who aren't accustomed to noticing internal body sensations.
For these clients, I recommend starting with body-based techniques first, then gradually introducing breath work once their nervous system feels more regulated.
Three Breathing Techniques That Work
Diaphragmatic Breathing (Belly Breathing) - Place one hand on your chest, one on your belly. Breathe in through your nose for 4 counts - your belly should rise while your chest stays relatively still. Exhale slowly through your mouth for 6 counts. The longer exhale activates your vagus nerve more powerfully than the inhale.
Box Breathing (4-4-4-4 Pattern) - Breathe in for 4 counts, hold for 4, exhale for 4, hold for 4. Repeat for 2-3 minutes. This technique creates rhythm that your nervous system can synchronize with, making it particularly effective when your mind is racing.
4-7-8 Breathing - Inhale through your nose for 4 counts, hold for 7, exhale completely through your mouth for 8. The extended hold and exhale force a deeper parasympathetic response. Many clients report feeling sleepy after just three rounds - this works well before bed.
When to Use Which Pattern
| Situation | Best Technique | Why It Works |
|---|---|---|
| Racing thoughts | Box breathing | Rhythm calms mental chatter |
| Physical tension | Diaphragmatic | Releases muscle tightness |
| Can't fall asleep | 4-7-8 | Produces drowsiness quickly |
| Moderate anxiety | Any of the three | All activate vagus nerve |
Common Mistakes
Breathing too slowly too soon. Start with your natural pace, then gradually extend the exhale. Forcing unnaturally slow breathing can trigger the paradoxical response.
Chest breathing instead of belly breathing. Shallow chest breathing keeps you in stress mode. Check that your belly expands on the inhale.
Practicing only when panicked. Your nervous system learns best when calm. Practice daily for 2-3 minutes when you're relaxed - then the technique becomes accessible during distress.
Giving up after one attempt. If breathing increases your anxiety, that's valuable information about your nervous system. Try a body-based approach first, then return to breath work later.
Dr. Alicia Meuret, psychology professor at Southern Methodist University, explains: "For individuals with panic disorder, standard slow breathing can actually trigger panic attacks because it changes their CO2 levels in ways their bodies interpret as dangerous."
This is why technique matching matters more than technique mastery.
Body-Based Calming Techniques
Your nervous system has a brake pedal.
Dr. Stephen Porges' polyvagal theory explains that your vagus nerve acts as this brake - when activated, it shifts you from fight-or-flight into a calm, connected state. The techniques below work by pressing that brake through your body rather than your mind.
These approaches are particularly powerful if thinking your way through distress feels impossible, or if you've experienced trauma or chronic stress that leaves you feeling disconnected from emotions.
Bilateral Tapping (Butterfly Hug)
Cross your arms over your chest with hands resting on opposite shoulders. Alternate tapping left, then right, slowly and rhythmically for 2-3 minutes.
This bilateral stimulation - borrowed from trauma therapy - calms your nervous system by engaging both brain hemispheres. Research shows this technique reduces emotional distress by 27-51% across studies, with many people reporting noticeable calm within 60 seconds.
Vagal Toning Methods
These techniques directly stimulate your vagus nerve:
Humming or singing: The vibration in your throat activates vagal fibers. Try humming for 30 seconds - you'll likely feel a shift in your chest tension.
Cold water on your face: Splash cold water or hold an ice pack to your face for 30 seconds. This triggers the "dive reflex," immediately slowing your heart rate by up to 13%.
Gargling: Gargle water vigorously for 30 seconds. The throat muscle activation stimulates the vagus nerve mechanically.
Progressive Body Scan
Lie down or sit comfortably. Starting at your toes, notice sensations in each body part without trying to change them - just observe temperature, tension, tingling.
Move slowly up through feet, calves, thighs, torso, arms, neck, face. This redirects attention from anxious thoughts to neutral body awareness, interrupting the distress loop.
Grounding Through Sensation
Hold a cold object, squeeze a textured item, or press your feet firmly into the floor. The key is intensity - strong physical sensations anchor you in the present moment when your mind is spiraling.
Try carrying a small stone or fidget item you can grip when anxiety rises.
Body-First vs. Cognitive-First: A Clinical Pattern
Through years of emotion-focused therapy, I've observed that people tend to fall into two categories: body-first and cognitive-first regulators.
Body-first people need somatic techniques to calm their nervous system before their thinking brain can engage. If you've experienced trauma, chronic stress, or feel emotionally numb, you likely need body-based approaches first.
Cognitive techniques become accessible only after your nervous system downregulates. If thinking through your anxiety feels impossible, that's not weakness - it's your signal to start with your body.
Dr. Pat Ogden, founder of the Sensorimotor Psychotherapy Institute, explains: "Trauma doesn't just create problematic thoughts - it creates problematic physical responses that operate beneath conscious awareness. For clients with significant trauma histories, the body must be engaged directly."
Using Movement to Calm Down
Not all movement calms you down.
The type of physical activity that helps depends entirely on your emotional state. What releases anger can amplify anxiety. What grounds anxiety can leave anger simmering.
Research shows this distinction clearly: a single 20-minute bout of moderate exercise reduces anger by 25-30% immediately, while anxiety reduction peaks 2-4 hours after movement. The timing difference reveals fundamentally different nervous system needs.
Anger Needs Controlled Release
Picture the restlessness after a heated argument - your body is flooded with adrenaline that demands discharge.
Anger requires intense physical outlets: sprinting, heavy bag work, resistance training, or high-intensity intervals. These activities provide structured channels for explosive energy without reinforcing aggressive patterns.
What NOT to do: Punching walls, slamming doors, or uncontrolled aggressive expression actually strengthens anger neural pathways. Your brain learns to associate rage with violence, making future episodes more likely.
Through my work with Contextual Anger Regulation Therapy (CART), I've observed a critical pattern: anger often needs brief, intense physical release through controlled outlets.
Think 10-15 minutes of heavy bag combinations or sprint intervals - enough to discharge the adrenaline surge without exhausting yourself. The structure matters as much as the intensity.
Anxiety Needs Gentle Grounding
Sunday evening anxiety spirals require the opposite approach.
Anxiety responds to rhythmic, moderate-intensity movement: walking, gentle cycling, swimming, or yoga. These activities calm your nervous system rather than activating it further.
Here's what surprises most people: high-intensity exercise worsens anxiety for roughly 30% of people during the activity itself. When your sympathetic nervous system is already on high alert, intense cardio can feel like adding fuel to a fire.
Dr. Matthew Stults-Kolehmainen, exercise psychology researcher at Yale University, explains: "Pushing an already anxious person into high-intensity exercise can backfire dramatically, essentially asking their nervous system to do more of what's already overwhelming them."
Matching Movement to Your State
| Emotional State | Movement Type | Why It Works |
|---|---|---|
| Anger/rage | 10-15 min intense (sprints, heavy bag, HIIT) | Discharges adrenaline through controlled channel |
| Anxiety/panic | 20-30 min moderate (walking, gentle cycling) | Activates calming without amplifying arousal |
| Mixed distress | Mind-body practices (yoga, tai chi) | Combines movement with breath awareness |
The key is recognizing which emotional state you're in before choosing your movement approach. Getting this match wrong can leave you feeling worse rather than better.
Grounding Techniques for Anxiety
When thoughts spiral - replaying yesterday's mistake or catastrophizing tomorrow's presentation - your body tenses in response to mental content, not present reality. Grounding techniques interrupt this loop by redirecting attention to concrete sensory information happening right now.
Research shows that systematic sensory engagement reduces acute anxiety more effectively than trying to engage all senses at once. Studies found sequential grounding helped 65% of people compared to 43% with simultaneous multi-sensory approaches.
The 5-4-3-2-1 Technique
This structured sequence forces your attention outward, one sense at a time:
Name 5 things you see - Look around slowly. Blue mug. Wooden chair. Silver doorknob. Green plant. Black phone. Say them aloud or silently, noticing colors and shapes.
Name 4 things you hear - Close your eyes if helpful. Hum of refrigerator. Traffic outside. Your own breathing. Distant voices. Notice volume and pitch.
Name 3 things you touch - Press your feet into the floor. Feel the texture of your shirt. Run your hand along the chair armrest. Focus on temperature and texture.
Name 2 things you smell - If nothing is obvious, notice air quality. Faint coffee scent. Clean laundry. Soap on your hands. Even neutral air counts.
Name 1 thing you taste - Sip water, chew gum, or simply notice the taste in your mouth right now.
The entire sequence takes 3-5 minutes. Move slowly through each sense - rushing defeats the purpose.
Other Sensory Grounding Methods
Cold objects: Hold ice cubes, splash cold water on your face, or grip a frozen water bottle. The intense sensation demands attention, pulling you from thought spirals.
Textured items: Carry a smooth stone, rough fabric, or ridged fidget object. Focus completely on how it feels - temperature, weight, surface texture.
Sounds: Play familiar music, listen to rain sounds, or focus on ambient noise. Naming three distinct sounds you hear grounds you in your environment.
Strong scents: Smell coffee, peppermint oil, or citrus. Scent processing bypasses your thinking brain, creating immediate sensory engagement.
When Grounding Works Better Than Breathing
Grounding shines when anxiety manifests as racing thoughts rather than physical symptoms.
If you're lying awake at 2am mentally replaying conversations, or sitting through a meeting while catastrophizing outcomes, your body isn't particularly activated - your mind is. Breathing techniques won't help because your nervous system isn't the primary problem.
People who describe themselves as "stuck in my head" typically respond better to grounding than body-based techniques. The external sensory focus provides an anchor when internal experience feels overwhelming.
While the 5-4-3-2-1 technique is widely recommended, my clinical experience suggests it works best for moderate anxiety and dissociative states. During severe panic when your prefrontal cortex is essentially offline, grounding may feel impossible to execute.
If you're trying to ground but can't focus on the steps, that's your signal to try body-based or movement approaches first. Once your nervous system calms slightly, grounding becomes accessible again.
Dr. Helen Kennerley, clinical psychologist at the University of Oxford, explains: "Grounding works by hijacking the attention system - when someone is anxious, their attention is often captured by internal threats. Sensory grounding provides external anchors that are neutral or positive, essentially giving the brain something safer to focus on."
Cognitive Techniques for Calming Nerves
What if your mind won't stop spinning?
When anxiety or anger lives primarily in your thoughts - replaying conversations, imagining worst outcomes, building cases about unfairness - cognitive techniques can interrupt these loops faster than body-based approaches.
But there's a critical limitation: cognitive strategies work best when your nervous system is regulated enough for your thinking brain to engage. If you're in full panic or rage, try body-based techniques first.
Who Benefits Most From Cognitive Approaches
Cognitive techniques work best when you:
Can identify the specific thoughts driving your emotion
Feel emotionally distressed but physically calm enough to think
Notice your mind catastrophizing or building resentment narratives
Respond well to logical analysis and perspective-taking
Experience anxiety more as worry than physical symptoms
Emotion Labeling: Name It to Tame It
The simplest cognitive intervention is naming what you feel.
Research shows that verbally labeling emotions - saying "I'm feeling anxious" or "This is anger" - reduces amygdala activity by 20-30% within seconds. Your brain's language centers automatically calm limbic reactivity when you put feelings into words.
Dr. Matthew Lieberman, professor of psychology at UCLA, explains the mechanism: "When you put feelings into words, you're activating the prefrontal cortex and reducing the response in the amygdala. It's essentially a form of implicit emotion regulation - it works without conscious effort to regulate."
Try this: When distress rises, pause and complete this sentence aloud or in writing: "Right now, I'm feeling ___ because ___." The act of naming creates immediate distance.
Challenge Distorted Thinking
Your thoughts during distress aren't always accurate.
When someone criticizes your work in a meeting, your mind might immediately conclude: "They think I'm incompetent. I'll probably get fired. I've always been a failure."
Ask yourself these questions:
What's the evidence for this thought? What concrete facts support it versus assumptions I'm making?
What's an alternative explanation? What are three other reasons this situation might have occurred?
What would I tell a friend? If someone I cared about had this thought, what would I say to them?
How likely is the worst outcome? On a scale of 1-100%, what's the realistic probability?
Will this matter in a year? What's the long-term significance of this situation?
These questions activate your prefrontal cortex, shifting you from emotional reactivity to analytical thinking.
Matching Cognitive Work to Your Emotional State
The pattern I consistently notice: anger focuses on others' wrongdoing, while anxiety focuses on your own feared inadequacy. This means the cognitive work differs entirely.
Anger requires examining fairness assumptions and intent attributions, while anxiety requires probability assessment and self-judgment challenging.
For anger: Ask "Am I reading malicious intent where none exists?" and "Is my rule about fairness realistic?"
For anxiety: Ask "How likely is this outcome really?" and "Can I handle this even if it happens?"
Quick Calming Strategies for Immediate Relief
Sometimes you need calm right now.
When you have 10 minutes during lunch to reset before an afternoon meeting, or you're wound up before bed and need sleep, these evidence-based techniques provide fast relief without requiring extended practice sessions.
Music and Sound (10-15 minutes)
Listen to slow-tempo music at 60-80 beats per minute - roughly matching your resting heart rate. Research shows this reduces anxiety by 30-35% within 10-15 minutes.
Classical music, nature sounds, or ambient tracks work best. Music with minimal lyrics proves more effective because language processing competes with relaxation mechanisms.
Nature Exposure (5-15 minutes)
Step outside, look at trees through a window, or watch nature videos. Even 5 minutes reduces cortisol by 13%, with effects increasing to 21% at 10-15 minutes.
Scenes with water or expansive views produce stronger stress reduction than enclosed spaces.
Progressive Muscle Relaxation - Quick Version (8-10 minutes)
Tense each major muscle group for 7-10 seconds, then release for 15-20 seconds. Start with your hands, move through arms, shoulders, face, stomach, legs.
The tension-release cycle signals safety to your nervous system through physical feedback.
Cold Water (30-60 seconds)
Splash cold water on your face or hold an ice pack to your face. This activates your vagus nerve within seconds, immediately slowing heart rate.
As covered in body-based techniques, this works through the dive reflex - an evolutionary stress-reduction response.
Verbalization with Support (5-10 minutes)
Call a trusted friend or family member and name what you're experiencing. Putting feelings into words reduces emotional intensity through the same emotion-labeling mechanism discussed in cognitive techniques.
Your prefrontal cortex calms limbic reactivity when you articulate distress.
Finding Your Go-To Strategies
Not every technique works for every nervous system.
Through years of helping clients build emotion regulation skills, I've observed that most people discover 2-3 favorite techniques that consistently work for their unique wiring. One person finds music transformative while another needs physical movement. Someone responds to cold water while their partner needs nature exposure.
This isn't random - it reflects genuine differences in how nervous systems respond to sensory input.
Dr. Matthew Stults-Kolehmainen, stress researcher at Yale University, explains: "These interventions work through biological mechanisms with optimal activation ranges. Too little intensity fails to trigger the response; too much can activate defensive systems. The sweet spot produces maximum benefit with minimal adverse effects."
Experiment when you're calm, not during crisis. Try each technique twice on different days. Notice which ones produce that subtle shift - shoulders dropping, breath deepening, mental chatter quieting.
Those are your go-to strategies. Keep them accessible for when overwhelm hits.
When These Calming Techniques Aren't Enough
You've practiced breathing exercises for three weeks. You've tried grounding. You've downloaded meditation apps.
Nothing helps.
Here's what most advice won't tell you: consistent technique practice that produces no improvement isn't a personal failure - it's valuable information that you're dealing with something requiring professional support.
Acute Distress vs. Chronic Dysregulation
Research shows a clear timeline distinction.
Acute stress - triggered by specific life events like job loss or relationship conflict - typically responds to self-help techniques within 2-4 weeks of consistent practice. You notice your anxiety decreasing, anger episodes becoming less frequent, or sleep improving.
When symptoms persist unchanged beyond 6-8 weeks despite genuine technique practice, you've crossed into territory that almost always requires professional treatment. Studies found that only 15-20% of people in this category eventually improve through continued self-help alone.
The difference isn't about trying harder. It's about underlying causes - unprocessed trauma, learned nervous system patterns, neurological factors, or clinical conditions - that need specialized intervention.
Signs You Need Professional Support
Seek therapy when you notice:
Symptoms preventing basic functioning - you're missing work, avoiding relationships, or struggling with self-care for more than two weeks
Functional impairment across multiple areas - when distress impacts work AND relationships AND daily activities, research shows 85% accuracy in predicting treatment necessity
Techniques making things worse - increased panic during breathing exercises, more anger after attempting cognitive work, or heightened anxiety from relaxation attempts
Symptoms worsening over time - escalating frequency, intensity, or duration despite your efforts
Suicidal thoughts, self-harm urges, or substance use as coping - these require immediate professional assessment
New avoidance behaviors - you're restricting activities, avoiding people, or creating safety rules that shrink your life
After working with 500+ therapy clients struggling with anxiety and anger, I've learned to recognize when self-help techniques aren't enough.
If you're practicing these approaches consistently but still experiencing persistent symptoms that impact your work, relationships, or daily functioning, that's not a failure of willpower.
It's a sign that you're dealing with something requiring professional support. Chronic anxiety or anger often has underlying causes - unprocessed trauma, learned patterns, neurological factors - that therapy addresses at a deeper level than technique practice alone can reach.
Dr. David Barlow, founder of the Center for Anxiety and Related Disorders, explains: "The clearest distinction isn't symptom intensity but response trajectory and functional impact. If someone practices evidence-based techniques consistently for 4-6 weeks and sees no improvement - or sees worsening - that's a red flag."
You're Not Broken - You Might Just Need Different Support
Needing professional help doesn't mean techniques failed.
It means your nervous system requires the kind of regulation support, trauma processing, or pattern interruption that happens in therapeutic relationships. Many conditions - panic disorder, PTSD, chronic anger patterns, complex trauma - respond minimally to self-help regardless of practice quality.
Therapy provides what self-help cannot: personalized assessment, technique matching to your specific nervous system, processing of underlying causes, and relationship-based nervous system regulation.
If you're in Calgary and these techniques aren't providing the relief you need, specialized support is available. Contact Emotions Therapy Calgary for a consultation to discuss how professional treatment can help.
Crisis support: If you're experiencing thoughts of harming yourself or others, call 988 (Suicide & Crisis Lifeline) or go to your nearest emergency room. You don't have to face this alone.
Conclusion
You now have a comprehensive toolkit.
The key insight: calming down isn't about finding the "right" technique that works for everyone. It's about understanding your unique nervous system and matching strategies to your specific emotional state.
Research on emotion regulation confirms this: the most successful people don't master one technique - they develop a small repertoire of 2-3 approaches that consistently work for their nervous system, then practice using them in real situations.
Start Here
To build your calming skill set:
Choose 2-3 techniques that feel most accessible right now. Pick from different categories - maybe one breathing approach, one body-based method, one cognitive strategy. This gives you options when one approach isn't working.
Practice when you're calm, not just during crisis. Studies show that practicing techniques during moderate stress (not just when relaxed) increases your ability to use them when you genuinely need them by 73%. Try them during low-stress moments first, then gradually during more challenging situations.
Track what actually works for your nervous system. Notice which techniques produce that subtle shift - shoulders dropping, breath deepening, mental chatter quieting. Those are your go-to strategies.
Give techniques 2-4 weeks of consistent practice before deciding. Most emotion regulation skills show meaningful effects within this timeframe, though full automaticity takes 8-12 weeks.
Through my clinical work, I've observed that most people eventually identify 2-3 favorite techniques that become their default calming strategies. One client might discover that cold water and walking work reliably, while another finds bilateral tapping and box breathing most effective.
This discovery process is valuable. What works for your nervous system isn't random - it reflects genuine physiological compatibility between technique and your stress response patterns.
If These Techniques Aren't Enough
Consider therapy when:
You've practiced techniques consistently for 6-8 weeks with minimal improvement
Symptoms prevent you from functioning at work, in relationships, or with basic self-care
Emotional difficulties are worsening despite your efforts
You're developing new avoidance behaviors that restrict your life
You're experiencing suicidal thoughts, self-harm urges, or using substances to cope
If you're in Calgary struggling with persistent anxiety or anger, Emotions Therapy Calgary offers specialized support including anger management therapy, anxiety treatment, and emotion-focused therapy. Contact us for a consultation.
Crisis support: If you're experiencing thoughts of harming yourself or others, call 988 (Suicide & Crisis Lifeline) or go to your nearest emergency room immediately. You don't have to face this alone.